Hypertension and prostanoid signaling in the subfornical organ of the brain
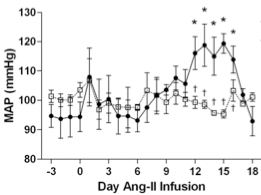
- Our work shows that excessive Ang-II type-1 receptor (AT1R) activation and NADPH oxidase (Nox)-dependent reactive oxygen species (ROS) signaling in the subfornical organ (SFO) are critical in "slow-pressor" Ang-II hypertension, a chronic Ang-II infusion model that recapitulates critical features of essential hypertension. However, the mechanisms by which Ang-II and oxidant stress in the SFO lead to adaptive changes in downstream neural pathways controlling blood pressure and volume homeostasis remain unknown.
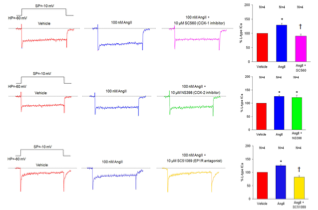
- Cyclooxygenase (Cox)-derived prostanoids have been implicated in Ang-II hypertension, and roles for prostaglandin E2 (PGE2) and PGE2 type-1 receptors (EP1R) have recently emerged. However, the source of PGE2 (Cox1 or Cox2) and its site(s) of action have not been defined.
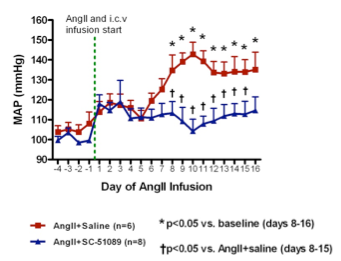
- Our preliminary results suggest an important role for PGE2 in Ang-II signaling in the SFO. Suppression of PGE2 signaling markedly attenuates both central Ang-II-induced drinking responses and increases in voltage-gated Ca2+ currents in SFO neurons. Furthermore, EP1R inhibition attenuates Ang-II-induced ROS formation in SFO neurons, and "slow-pressor" Ang-II hypertension is prevented in EP1R null mice.
- Based on these findings, we are employing molecular, neurophysiological, neuroanatomical and integrative cardiovascular physiological analyses to test the central hypothesis that Cox1-derived PGE2 provides an essential link between Ang-II, ROS and the adaptive changes that occur in the CNS and that lead to neurohumoral dysfunction and hypertension in the Ang-II "slow-pressor" model.