Human Health
Where can I find out about human cases of HPAI?
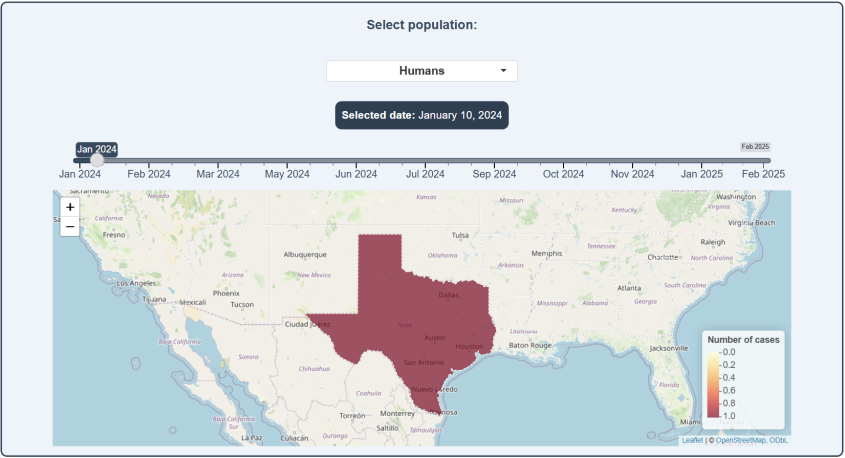
Although rare, there is a risk of human infection from frequent or heavy exposure to infected animals. The Centers for Disease Control (CDC) reports updated numbers of infections in humans linked to the ongoing H5N1 outbreak. Thus far, there has been one death, representing <2% of known cases.
What puts me at risk of being infected?
The primary risk factor for human infection is exposure to infected poultry, wildlife and dairy cattle, or to contaminated environments. Importantly, the animal does not have to be alive to pose a risk of zoonotic (from animal to person) transmission. Therefore, slaughtering, de-feathering and handling of carcasses are all risk factors for contracting infection.
The CDC states that, because of their routine contact with animals, individuals who work on farms, or closely with domestic animals or wildlife – whether backyard poultry owners, veterinarians or those with recreational exposures – are at increased risk. Health care providers and emergency responders are also at increased risk due to their potential contact with infected people.
Can I become infected from food?
There is currently no evidence suggesting transmission through consumption of properly prepared and cooked poultry, eggs or other animal products.
However, there is a risk of transmission through the consumption of raw contaminated products, such as raw milk from an infected dairy cow or cheeses made from raw milk. It is highly recommended that neither people nor their pets eat raw animal-source foods or raw milk products.
NYS recommends cooking poultry and eggs to 165 degree internal temperature.
If you are concerned you have been exposed to avian influenza and are feeling unwell, please consult your primary care provider.
If I do handle animals, how can I reduce my risk of infection?
Personal protective measures are essential in limiting exposure to HPAI, especially among those who are at a higher risk.
Preventative measures include:
- Regular hand washing
- Covering your mouth and nose when coughing or sneezing
- Self-isolation of those feeling unwell
- Avoiding close contact with people and animals that are showing signs of illness
- Wearing personal protective equipment if avoidance of symptomatic individuals or infected animals is not possible, or if you're working with large numbers of potentially sick animals
- Correct handling of potentially infected animals, including when disposing of dead birds, depopulating flocks and interacting with animal carcasses from hunting or while butchering. More on this topic can be found on in our Wildlife Resource page.
If the number of human cases is still low, and there is currently no evidence of transmission from person-to-person, why does HPAI seem to be generating so much concern?
Apart from potentially directly causing illness in people, HPAI is currently causing billions of dollars of losses to the agricultural industry in the United States, and this has important impacts on the price of food and overall economy, both of which affect our health.
As important as the economic losses are, we must also be very cautious with influenza viruses because of their ability to evolve. Although the virus does not currently have the ability to be transmitted from person to person, public health officials are concerned that it could quickly develop that capability through mutation or mixing with other flu viruses, which could lead to rapid spread in people.
Some trusted resources for further information
- For more information on the signs and symptoms of bird flu, visit the signs and symptoms page of the CDC and an update from the American Medical Association.
- For up-to-date information about the current outbreak, visit the Current Situation page from the CDC and the Avian Influenza page from the USDA.
- For information on disease outbreaks of interest to public health around the world, visit New York State’s Department of Health Global Health Update.
This page was last updated on Tuesday, Mar 18, 2025