Enzyme-armed immune cells serve as early defense against tuberculosis infection
Researchers have discovered a specific class of immune cells that can be harnessed to fight tuberculosis in its earliest stages. The finding, published Sept 24 in Nature Communications by Dr. David Russell, the William Kaplan Professor of Infection Biology in the Department of Microbiology and Immunology, describes how the immune cells known as CD38+ macrophages play a vital role in fighting early infection in the lung by Mycobacterium tuberculosis (Mtb), the bacteria responsible for tuberculosis.
Russell and colleagues have previously found that that certain macrophages either control or promote an Mtb infection. “Understanding the specific role of these macrophages during Mtb infection is key to uncovering disease mechanisms and guiding the development of effective vaccines,” says Russell.
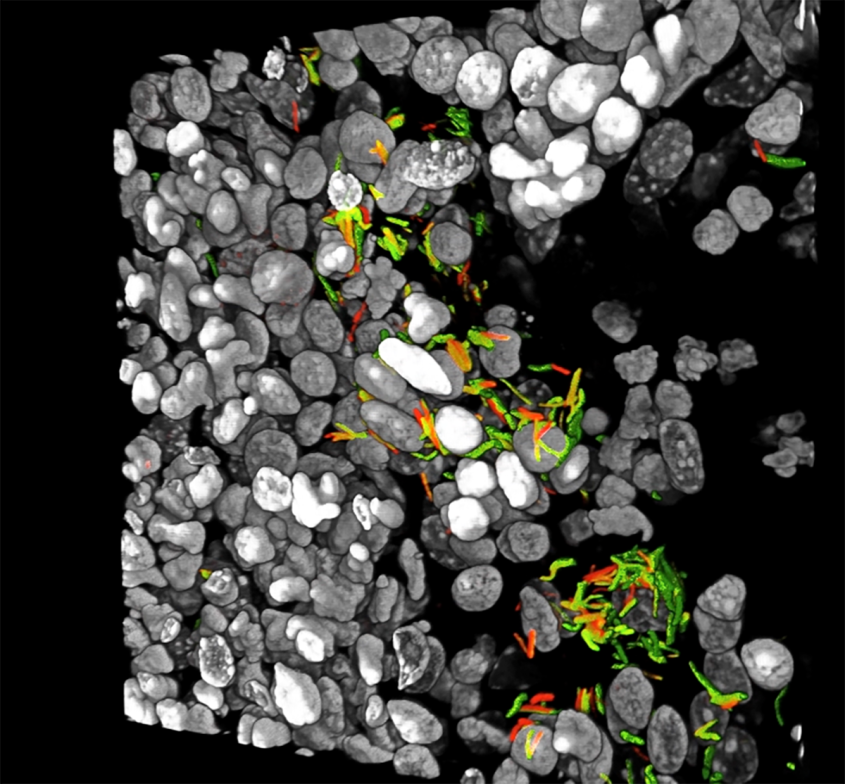
Since their earlier discovery, Russell’s team has looked even more closely at how particular macrophages react to Mtb infection, developing a new technique known as multi-modal single-cell RNA sequencing, or scRNA-seq. This method analyzes the RNA transcripts of individual cells, and links those host cell transcripts to “reporter” Mtb bacteria that glow different colors depending on how stressed they are in their environment. Using this approach, the researchers could get a genetic read-out of individual immune cells along with visual proof of how the Mtb bacteria fared in those host immune cells.
Russell leveraged his high-tech method in this most recent study to examine a subset of immune cells known as CD38+ macrophages. Their name refers to the elevated levels of an enzyme called CD38, which is known to help restrict infections by boosting the body’s inflammatory response.
To better understand how these macrophages behaved in vivo, scientists exposed mice to Mtb infection and tracked how their different lung immune cells reacted over time. Macrophages lacking the CD38+ enzymes were the first to be attacked by the bacteria and succumbed quickly to the Mtb. Fortunately, however, their CD38+ macrophage counterparts soon came to the rescue, fighting back against the Mtb intruders with their inflammation-fueling enzymes. “These CD38+ macrophages help transform the lung environment into a pro-inflammatory state, effectively curtailing Mtb growth,” Russell says.
The researchers next investigated how the CD38+ macrophages in healthy mice reacted when given a TB vaccine. They found that the vaccine boosted the numbers of these Mtb-fighting immune cells, posing promise for future therapies. “The changes in macrophage populations after immunization provided insights into potential strategies for reprogramming these macrophages to our advantage,” says Russell. “While our mouse studies do not fully capture the complex genetic and environmental influences found in humans, the changes in macrophages we observed during infection and after vaccination offer a tractable path towards improved TB control.”
Written by Lauren Cahoon Roberts